- Home
- News
- Spotlight on Science
- Unexpected tolerance...
Unexpected tolerance of the spinal cord to X-ray microbeams
02-07-2013
Microbeam radiation therapy (MRT) could one day be used to treat tumours in or around the spinal cord. Studies at the ESRF’s biomedical beamline demonstrate that this technique can be used to deliver a higher radiation dose than a conventional X-ray beam before damage to normal tissues becomes apparent. The effect of MRT on rat cervical spinal cord was compared to irradiation from a “wide” X-ray beam. Long-term behavioural studies and histological scrutiny of the lesions revealed that spinal tissues have an unexpected high tolerance of microbeams.
Investigation of MRT for the palliation/ablation of malignant cancers at radiosensitive neurologic and ophthalmologic sites, particularly in very young individuals, were initiated in the 1990s and are now one of the main research avenues of the ESRF’s biomedical beamline, ID17.
The therapeutic index for MRT, i.e., the index for the maximum dose that produces acceptable normal-tissue damage, divided by the minimum dose that controls the tumour, has been shown to outdo therapeutic indices achieved by conventional wide single beams. This advantage is largely due to the high tolerance of the brain, the skin and other organs to a radiation dose in the hectogray range if delivered by microbeams. Radio-oncologists familiar with the concept deem that MRT, if validated in preclinical safety studies in large animals, might enable the palliation of malignant tumours in the brain of infants and young children which, at present, cannot be safely and effectively treated [1]. In the present work, we asked whether similar tumours located in or around the spinal cord could also be amenable to MRT.
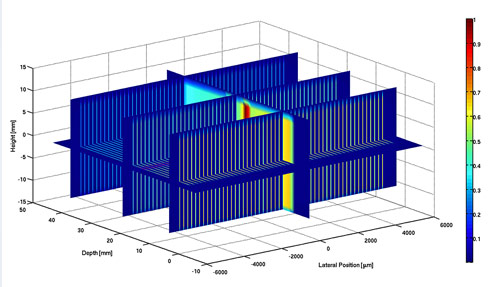
To address this question, a multinational team has studied the tolerance and late dose-related responses of the cervical spinal cord of rats to synchrotron X-rays by irradiating it once, using an array of 35 micron wide, parallel, vertical X-ray microbeams (“peaks”), separated by 175 micron-wide, nominally non-irradiated “valleys” (Figure 1). The segment of the cervical spinal cord, irradiated transversely, was 11 mm long. Comparison was made with rats irradiated with a single, only 1.35 mm “wide” beam of similar X-rays. The rats lived until paralysis began to develop.
Results
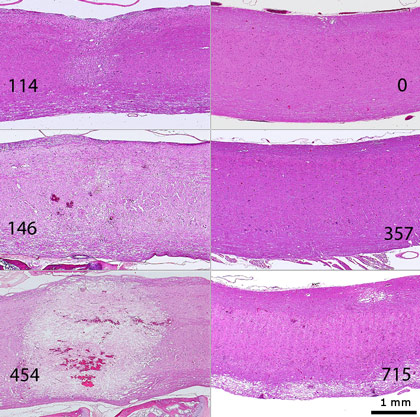
Microbeams: Peak/valley doses of 507/18 Gy and 715/25.4 Gy elicited foreleg paralysis around 60 days after irradiation. Conversely, 8 of 10 rats exposed to peak/valley doses of 357/12.7 Gy, and all rats exposed to peak/valley doses of 253/9 Gy were paralysis-free at 383 days after irradiation. The computed dose that would cause paralysis in 50% of the rats, the so-called ED50, was 373.3 Gy (peak), and 13.2 Gy (valley).
Single “wide” beam: The ED50 was ≈3 times lower than for microbeams, 130.1 Gy, delivered to a very short (1.35 mm) segment of the cervical spinal cord. After doses of 146 or 454 Gy all rats developed paralysis by 1.5 or 2 days after irradiation, respectively, but all rats exposed to 57 or 114 Gy survived up to 230 days after irradiation without paralysis.
Histopathologically, the damage to cervical spinal cord tissues was much more severe in rats exposed to a single “wide” beam, where doses ≥ 146 Gy destroyed normal tissues (=necrosis), than in rats exposed to microbeams (Figure 2).
The peak dose that would cause paralysis in 50% of the rats, 373 Gy delivered by microbeams to any segment of the mammalian spinal cord, is the highest ever reported, to our knowledge. MRT peak doses in the same range have been used for the palliation/ablation of brain tumours in rats and other animals and might thus also be applied to the spinal cord.
Principal publication and authors
Response of the rat spinal cord to X-ray microbeams, J.A. Laissue (a), S. Bartzsch (b), H. Blattmann (a), E. Bräuer-Krisch (c), A. Bravin (c), D. Dalléry (c), V. Djonov (a), A.L. Hanson (d), J.W. Hopewell (e), B. Kaser-Hotz (f), J. Keyriläinen (g), P. Philippe Laissue (h), M. Miura (d), R. Serduc (i,j), A.E. Siegbahn (k), D.N. Slatkin (l), Radiotherapy and Oncology 106, 106–111 (2013).
(a) University of Bern (Switzerland)
(b) DKFZ, Heidelberg (Germany)
(c) ESRF
(d) Brookhaven National Laboratory, NY (USA)
(e) University of Oxford (UK)
(f) Animal Oncology and Imaging Center, Hünenberg (Switzerland)
(g) Helsinki University Central Hospital (Finland)
(h) University of Essex, Colchester (UK)
(i) INSERM, U836, Grenoble (France)
(j) Université Joseph Fourier, GIN, Grenoble (France)
(k) Karolinska University Hospital, Stockholm (Sweden)
(l) Nanoprobes, Inc., Yaphank NY (USA)
References
[1] J.A. Laissue, H. Blattmann, H.P. Wagner, M.A. Grotzer, D.N. Slatkin, Dev Med Child Neurol 49, 577–81 (2007).
Top image: Microbeams are used to deliver a high radiation dose to a target while mimimising damage to surrounding normal tissues.