- Home
- Users & Science
- Scientific Documentation
- ESRF Highlights
- ESRF Highlights 2006
- X-ray Imaging and Optics
- Differences in the time course of proximal and distal airway response to inhaled histamine studied by synchrotron radiation CT
Differences in the time course of proximal and distal airway response to inhaled histamine studied by synchrotron radiation CT
Quantitative study of lung function with synchrotron radiation is a long-term project conducted at the Biomedical Beamline, ID17. The goal of the project is to understand the effects of drugs and air pollutants in healthy and diseased lung, and find optimal medication for such common diseases as asthma. The project is based on collaboration between teams working at the ESRF, University of Helsinki, Université de Picardie, Szeged University (Hungary), and Geneva University Hospital.
Stable Xe gas is used as the inhaled contrast agent for imaging the airspaces of an animal model (rabbit). Two simultaneous images are recorded using two X-ray energies that bracket the K-absorption edge of Xe, and the difference image in a logarithmic scale yields the distribution of the contrast gas. The spatial resolution determined by the beam height and detector resolution is 0.1 mm3, which is more than an order of magnitude better than the resolution achieved by any other method for lung imaging. In addition, the noise level is strongly reduced, as the signal from other parts of the object is eliminated.
Although airway hyperreactivity is the hallmark of bronchial asthma, little is known about the differences in the regional kinetics of airway narrowing in the tracheo-bronchial tree during an asthma attack. Previous studies in this project showed that inhaled histamine induces large patchy defects in Xe wash-in in the peripheral lung air spaces with rapid spontaneous reversal, suggesting that the in vivo reactivity and kinetics of airway response to histamine inhalation could be different in distal vs. proximal airways [1]. In this study the narrowing of proximal airways was imaged directly, while the distal airway obstruction was indirectly quantified by measuring changes in the regional ventilated area on the basis of the densities of Xe gas.
 |
|
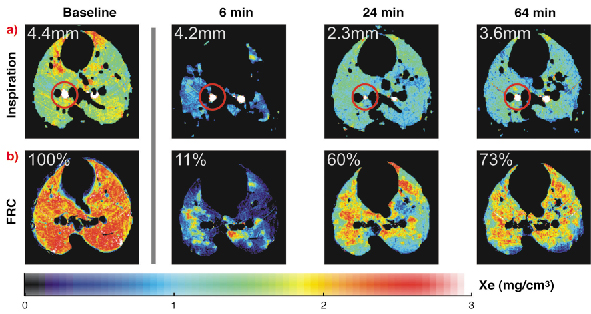
Fig. 127: Xe distribution in the middle lung cross-section level at baseline and 6, 24, and 64 minutes after histamine inhalation in a rabbit. a) changes in proximal airway caliber. One bronchus in the inspiration images is marked with a circle. The diameter of this bronchus is 4.4 mm in the baseline image; 6 minutes after histamine the diameter is 4.2 mm. The minimal diameter value of 2.3 mm is reached 24 minutes after the histamine inhalation, and recovery to 4.2 mm value is observed 64 minutes later. b) changes in the ventilated alveolar area at FRC, functional residual capacity. At 6 minutes after histamine inhalation the ventilated alveolar area is reduced to 11% of the baseline value with significant heterogeneity. The ventilated alveolar area recovered in 24 minutes to 60% of the baseline value and in 64 min to 73% of the baseline values. |
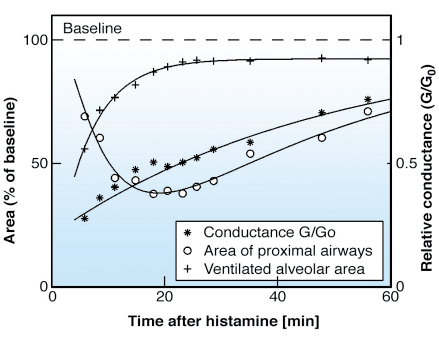
Results of the study are shown in Figure 127 and 128. The CT images show the slow contraction of a large airway, the immediate constriction of distal airways based on the reduction of the ventilated alveolar area, and the very non-uniform distribution of the ventilated air spaces in the lungs. The subsequent time course of lung response in Figure 128 shows the rapid recovery of the distal airways, and the slow recuperation of the main bronchi. A plausible explanation is that of different airway wall structures, as the relative cartilage content decreases and the smooth muscle content increases in distal airways. There are also indications that the delayed maximal response to histamine and the slow recovery observed in the main bronchi may be due to sub-mucosal edema formation followed by gradual removal.
 |
|
Fig. 128: Relative changes in respiratory system conductance G/G0, luminal area of proximal airways at the lower cross-section level where the largest response to histamine was observed, and ventilated alveolar area after inhalation of histamine aerosol. |
One of the most important overall indicators of lung function is the conductance (inverse of resistance) of the respiratory system. The findings of this study suggest that the changes in conductance result from combined reactions of proximal and distal airways. However, the relative contribution of these components seems very unequal in time after an asthma attack provoked by histamine. These findings are potentially important for studies of the patho-physiology and treatment of asthma.
References
[1] S. Monfraix, S. Bayat, L. Porra, G. Berruyer, C. Nemoz, W. Thomlinson, P. Suortti, A.R.A. Sovijärvi, Phys. Med. Biol., 50, 1-11 (2005).
Principal Publication and Authors
S. Bayat (a), L. Porra (b), H. Suhonen (b), C. Nemoz (c), P. Suortti (b,c), A.R.A. Sovijärvi (d), J. Appl. Physiol., 100, 1964-1973 (2006).
(a) Université de Picardie, Amiens (France)
(b) University of Helsinki (Finland)
(c) ESRF
(d) Helsinki University Central Hospital (Finland)



